
Both acetabular undercoverage (hip dysplasia) and overcoverage (pincer-type femoroacetabular impingement) can result in hip osteoarthritis. In contrast to undercoverage, there is a lack of information on radiographic reference values for excessive acetabular coverage.
(1) How do common radiographic hip parameters differ in hips with a deficient or an excessive acetabulum in relation to a control group; and (2) what are the reference values determined from these data for acetabular under- and overcoverage?
We retrospectively compared 11 radiographic parameters describing the radiographic acetabular anatomy among hip dysplasia (26 hips undergoing periacetabular osteotomy), control hips (21 hips, requiring no rim trimming during surgical hip dislocation), hips with overcoverage (14 hips, requiring rim trimming during surgical hip dislocation), and hips with severe overcoverage (25 hips, defined as having acetabular protrusio). The hips were selected from a patient cohort of a total of 593 hips. Radiographic parameters were assessed with computerized methods on anteroposterior pelvic radiographs and corrected for neutral pelvic orientation with the help of a true lateral radiograph.
All parameters except the crossover sign differed among the four study groups. From dysplasia through control and overcoverage, the lateral center-edge angle, acetabular arc, and anteroposterior/craniocaudal coverage increased. In contrast, the medial center-edge angle, extrusion/acetabular index, Sharp angle, and prevalence of the posterior wall sign decreased. The following reference values were found: lateral center-edge angle 23° to 33°, medial center-edge angle 35° to 44°, acetabular arc 61° to 65°, extrusion index 17% to 27%, acetabular index 3° to 13°, Sharp angle 38° to 42°, negative crossover sign, positive posterior wall sign, anterior femoral head coverage 15% to 26%, posterior femoral head coverage 36% to 47%, and craniocaudal coverage 70% to 83%.
These acetabular reference values define excessive and deficient coverage. They may be used for radiographic evaluation of symptomatic hips, may offer possible predictors for surgical outcomes, and serve to guide clinical decision-making.
Level III, diagnostic study.

Avoid common mistakes on your manuscript.
Both acetabular undercoverage (developmental dysplasia of the hip [DDH]) and overcoverage (such as “pincer”-type femoroacetabular impingement [FAI]) can lead to degenerative hip arthritis. A different pathomechanism for each of these two conditions is supposed. Undercoverage may cause higher joint contact pressures [12] and subsequent degeneration of the articular cartilage resulting from static overload [13, 20]. Acetabular overcoverage may lead to early pathological contact between the overcovering acetabulum and the femoral head-neck junction [11]. This can lead to prearthrotic chondrolabral damage as a result of a more dynamic conflict at the acetabular rim [30].
Although acetabular undercoverage has been quantified before [5, 20, 34], there is a lack of information in the literature on excessive coverage. To our knowledge, an anatomically based quantification of overcoverage has never been explicitly described.
We therefore asked: (1) how do common radiographic hip parameters differ between hips with a deficient or excessive acetabulum in comparison to a control group; and (2) what are the anatomically based reference values for acetabular under- and overcoverage?
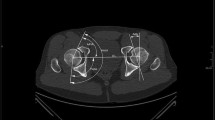
We performed a retrospective comparative study including a total of 86 selected, nonconsecutive nonarthritic hips (Table 1). We compared the radiographic anatomy of the acetabulum among four groups: a “dysplastic,” “control,” “overcoverage,” and “severe overcoverage” group. The allocation to each group (Fig. 1) was based on established radiographic criteria and direct visual inspection of the type of impingement conflict during surgical hip dislocation [9]. The “dysplastic” group consisted of a consecutive series of patients undergoing periacetabular osteotomy (PAO) [10] in 2004 (n = 59 hips). Inclusion criteria was a lateral center-edge (LCE) angle of ≤ 20° [20]. Exclusion criteria were improper/incomplete radiographs (n = 26) and hips with previous surgery (n = 26). The “control” and the “overcoverage” groups were recruited from 481 consecutive hips undergoing surgical hip dislocation for FAI (Fig. 1) [6]. Exclusion criteria were improper/incomplete radiographs (n = 260), previous hip surgery (n = 37), a history of pediatric hip disorder (n = 58), and hips with mixed cam-/pincer-type of FAI (n = 91). The remaining 35 hips either had isolated cam (n = 21 hips, “control” group) or pincer-type FAI (“overcoverage” group). The allocation to these two groups was based on the direct visual intraoperative dynamic assessment. The “control” hips only required a correction of the aspherical femoral head until impingement-free ROM was present during surgical hip dislocation. The “overcoverage” group only required isolated rim trimming without addressing the femoral head-neck junction. The “severe overcoverage” group consisted of hips with acetabular protrusio, which is established as the most severe form of pincer impingement. This group included hips in which the femoral head touches or crosses the ilioischial line on the AP pelvic radiograph [17, 32]. We excluded 26 hips with improper/incorrect radiographs and two hips with previous surgery from an initial cohort of 53 hips leaving 25 hips for the “severe overcoverage” group (Fig. 1). This retrospective comparative study was approved by the local institutional review board.
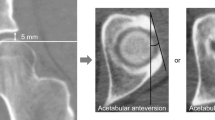
Two radiographic views acquired with a standardized technique were used for evaluation: an AP and a true lateral pelvic radiograph [32]. The AP radiograph was used to calculate the radiographic parameters; the true lateral radiograph was used to assess the individual pelvic tilt (described later). Both radiographs were taken consecutively without repositioning of the patient (Fig. 2). The film-focus distance was 120 cm for both views. For the AP pelvic radiograph, the center of the x-ray beam was directed to the midpoint of the symphysis and a line connecting the anterosuperior iliac spines. For the true lateral radiograph, the x-ray beam was centered on the tip of the greater trochanter.
We used previously validated and commercially available software (Hip 2 Norm [31, 33, 38]; University of Bern, Bern, Switzerland) for the evaluation of these radiographs. This software allows a reliable and reproducible evaluation of the most commonly used radiographic hip parameters. Repeatability statistics with use of this program have been published elsewhere [31]; briefly, the interobserver reliability and the intraobserver repeatability for the following chosen 11 parameters (Table 2) was good to very good (ie, intraclass correlation coefficient ≥ 0.61): LCE angle, medial center-edge angle, acetabular arc, extrusion index, acetabular index, Sharp angle, crossover sign, posterior wall sign, anterior femoral head coverage, posterior femoral head coverage, and craniocaudal femoral head coverage (Fig. 3). A special feature of Hip 2 Norm is the ability of correcting the radiographic parameters for tilt and rotation [33]. To exclude the influence of pelvic malpositioning, we calculate all radiographic value relative to a neutral pelvic orientation regarding tilt (around the transverse axis) and rotation (around the longitudinal axis). A neutral pelvic tilt was defined by a pelvic inclination of 60° [6, 19, 37]. This angle is formed by a horizontal line and a line connecting the upper border of the symphysis with the sacral promontory. This angle was measured on the lateral pelvic radiograph. A neutral pelvic rotation was defined when the center of the sacrococcygeal joint was aligned vertically with the middle of the pubic symphysis [33]. One observer (MT) assessed all radiographs.
Normal distribution was determined with the Kolmogorov-Smirnov test. Differences for demographic and radiographic data among the four study groups were determined with analysis of variance for continuous variables and the chi-square test for categorical variables. Reference values were derived from the intersection points of the normal distribution curves for each continuous variable. Reference values for categorical variables were determined by the highest prevalence in the control group.
All parameters except the crossover sign differed among the four study groups (Table 3). Of the nine evaluated continuous variables, five parameters (LCE angle, acetabular arc, AP/cranial coverage) increased steadily from dysplasia through control and overcoverage to severe overcoverage (Fig. 4). In contrast, four of the continuous parameters (medial center-edge angle, extrusion/acetabular index, Sharp angle) decreased from dysplasia to severe overcoverage.
The intersection of the normal distribution curves results (Fig. 5) in the formulation of characteristic thresholds for each continuous parameter. The following reference values were found: LCE angle 23° to 33°, medial center-edge angle 35° to 44°, acetabular arc 61° to 65°, extrusion index 17% to 27%, acetabular index 3° to 13°, Sharp angle 38° to 42°, negative crossover sign, positive posterior wall sign, anterior femoral head coverage 15% to 26%, posterior femoral head coverage 36% to 47%, and craniocaudal coverage 70% to 83% (Table 4).
In summary, based on direct intraoperative observation, we developed acetabular reference values for excessive and deficient coverage. These values can be used for radiographic evaluation of symptomatic hips, possible predictors of surgical outcomes, and as an adjunct for clinical decision-making. As shown in a previous study [29], the following parameters can be reliably measured without necessarily compensating for pelvic tilt and rotation on an AP pelvic radiograph (ie, without a true lateral radiograph): LCE angle, Sharp angle, acetabular and extrusion index, and craniocaudal coverage. Similar to what has been shown for the dysplastic hips [20], future studies need to investigate the natural course of hips with acetabular overcoverage. Despite the establishment of our preliminary guidelines, we emphasize that incidentally found abnormal radiographic values in asymptomatic patients are not an indication for surgery unless patients at risk would have been identified who will ultimately develop hip osteoarthritis.